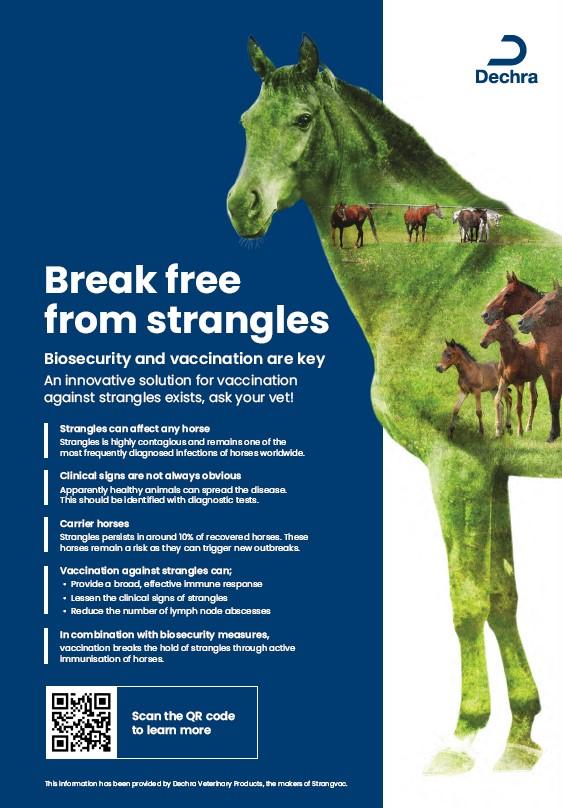
Horses travel around the world to attend equine events or sales, which creates a risk of transmission of infectious diseases worldwide. Recently, a global platform for genomic surveillance of Strep. equi was created and 670 isolates from 19 countries were examined. This unique project highlighted numerous examples of the transmission of Strep. equi around the world and the importance of biosecurity, diagnostic testing and vaccination for the prevention of disease transmission. The study identified six broad types of Strep. equi (BAPStypes), with emergence and dominance of BAPS2 in Europe.4